L. David Roper, http://www.roperld.com/personal/roperldavid.htm
26-May-2016
Around the year 2000 or earlier I started having numbness on the outside of my left thigh and my left buttock. Gradually it traveled down the leg and often a severe tingling pain would accompany it when standing for about 20 minutes or sometimes sitting for a long time. It hurts to sleep on either thigh, but especially the left one, and the buttocks sting when I sleep on the back and sit unless the bed or chair is very soft.
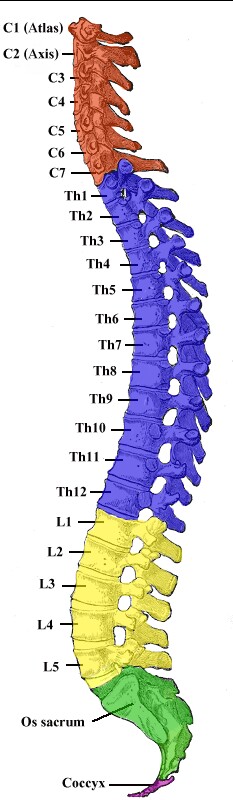
I saw a chiropractor in 2001 and had an x-ray taken of my lower spine. I saw a neurologist at Radford Hospital in May 2003 and had an MRI of my lower spine. The diagnosis was that I have bilateral spondylolysis at the L5 vertebra with mild spondylolisthesis. The L5 vertebra has slipped forward on the sacrum.
Since 2000 I have had three sets of 2 or 3 lumbar epidural steroid injections on the left side, which relieved the pain for a few years. The last set has lasted for several years. In 2014 I still have numbness on the outside of the left thigh and it stings badly when I stand for long periods; sitting down or walking stops the stinging quickly.
Because of right-hip pain an x-ray was taken on 12 March 2009: “Hip joint is symmetrical with the left hip. Small spurs are projecting in the superolateral aspects of the acetabula bilaterally. No other suspicious bony lesion is seen. IMPRESSION: Very mild degenerative changes.”
Before 2000 a rotator-cuff operation was done on the left shoulder.
Because of pain in my right shoulder x-rays were done on 9 April 2012 and 15 July 2013: “There is no fracture. There is no dislocation. There are faint calcifications noted in the superior aspect of the acromiohumeral joint inferior to the AC joint. There is also a spur formation from the anterior aspect of the acromion process measuring close to 5 mm, most likely resulting in impingement. There is minimal degenerative change involving the superolateral aspect of the humerus, compatible with chronic rotator cuff degenerative changes. Degenerative change at the AC joint is noted. Glenohumeral joint is preserved.
IMPRESSION: Spur formation from the acromion process and degenerative change of the acromioclavicular joint with probable impingement. Chronic rotator cuff degenerative tendinopathy. Calcific peritendinitis."
Nothing was done about it. The pain still occurs rarely.
15 July 2013: An x-ray was done on the left thumb because of sporadic pain: “There is narrowing with sclerosis and minimal spur formation at the first metacarpal phalangeal joint. There is a larger spur on the ulnar side of the first metacarpal carpal joint. Tiny spurs at the interphalangeal joint of the thumb. The MCP joint appears within normal. There are no joint erosions. There is no fracture or dislocation.
IMPRESSION: Degenerative arthritis, particularly the first metacarpal carpal joint.”
I started having sporadic tingling pain in my left arm and into the fingers. X-rays of my neck were done at Montgomery Hospital which indicated a pinched nerve in the neck due to arthritis of the spine. Nothing was done about it. The pain still occurs rarely.
24 March 2014: Because of pain in the left arm, at Montgomery Lewis Gale Hospital underwent resting nuclear imaging after receiving 15 mCi of Technetium Sestamibi . Then underwent exercise stress. Then received 42 mCi of Sestamibi and underwent gated nuclear imaging. The results were:
I have been having severe calf and foot cramps over the last year or so, mostly in the right leg. I have been eating a banana just before going to bed, which seems to help.
When I sit on firm seats both buttocks and thighs sting; this has been the case for several years. I use a memory foam pillow on my car and table seats.
Recently I have been having some balance problems. I often am uncertain about my balance when walking. I sometimes have difficulty walking a line. I have been doing an hour of Tai Chi once a week for about 15 years hoping that will help with my balance.
Dr. Ethan Colliver tested my body strength and found that my strength is good except that my hips’ muscle strength is low.
I sporadically have brief sharp pain in the left and right knees, usually apart but sometimes together. An x-ray was done for one of the knees and arthritis was seen. My personal physician stated that the joint was in good shape.
After some hip pain on the right side an x-ray was done and arthritis was seen. My personal physician stated that the joint was in good shape.
When I sit in a chair for a long time doing tasks, I get a dull pain about 2/3rds of the way down the back. I quit playing the bass trombone in Blacksburg Community Band partly because of that. Also, when I bend over to do something I get much pain in the middle back. When I am on the floor I find it difficult to get up on my feet. When taking baths I have some difficulty getting out of the tub, unless hand bars are available.
Due to back pain my GP, Dr. William Hendricks, referred me to Dr. Tejal Raju, a pain specialist in Christiansburg VA.
15 October 2014: Dr. Tejal Raju arranged for an MRI to be done for my spine at Radford Hospital: “ MRI lumbar spine without contrast
Clinical indication: Lumbar radiculopathy
Technique: Exam is performed on the 3 Tesla scanner with T1, T2, STIR sequences in various planes.
Comparison: MRI lumbar spine January 16, 2008 report.
Findings:
Bones: The vertebral body heights are maintained. There is no measurable listhesis. There are no suspicious marrow signal abnormalities.
Conus: Normal size, signal, position at T12-L1. There are small perineural cysts or arachnoid diverticuli at several of the upper neural foramina, T11-T12, T12-L1. These are not typically of any clinical significance.
Discs:
T11-T12: There is diffuse disc bulging with no central canal or foraminal stenosis.
T12-L1: There is mild diffuse bulging with no canal or foraminal stenosis.
L1-L2: There is disc height loss and diffuse disc bulging. There is facet hypertrophy. The facet hypertrophy is greater on the left which causes mild mass effect on the posterior left side of the thecal sac. Technically, there is no central canal stenosis. There is minimal narrowing of the right foramen. There is mild to moderate narrowing of the entrance of the left foramen mostly due to the facet hypertrophy.
L2-L3: There is disc dehydration, disc height loss and diffuse disc bulging. There is facet and ligamentum flavum hypertrophy. There is central spinal canal stenosis, moderate. There is mild bilateral foraminal narrowing.
L3-L4: There is marked disc height loss. There is diffuse disc bulging, facet and ligamentum flavum hypertrophy. There is circumferential spinal canal stenosis, moderate. There is right lateral recess stenosis, moderate to severe right foraminal stenosis and moderate left foraminal stenosis.
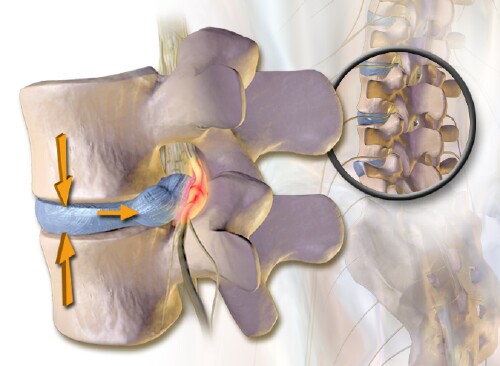
L4-L5: There is a disc extrusion on the right with disc material extending inferiorly, posterior to the upper margin of the L5 vertebra. There is displacement of the descending nerve roots. Additionally, there is diffuse disc bulging, facet and ligamentum flavum hypertrophy as well as small synovial cyst or associated with the right and left facet joints. These factors combine to cause moderate to severe central spinal canal stenosis. There is severe right foraminal stenosis due to a combination of these factors and mild to moderate left foraminal stenosis.
L5-S1: There is mild diffuse bulging. This is most prominent at the level the foramen with foraminal stenosis on the right causing some deformity of the nerve root within the foramen and to a lesser extent on the left side. Central canal is not stenotic.
Extraspinal: No significant findings in the field-of-view.
Impression:
1. Multilevel degenerative lumbar disc disease and facet arthritis.
2. Multilevel spinal canal and foraminal stenosis.
3. Disc extrusion on the right at the L4-L5 level.”
I had 2 epidural steroid injections by Dr. Tejal Raju for back pain in October/November 2014, which greatly helped so far.
I had a dull ache in my right hip/buttock area in November 2014. An epicural steroid injection was done by Dr. Tejal Raju on 10 November 2014; I felt a minor pain when the injection occurred.
Four days after that injection I started having major pain up and down the right leg. An epidural steroid injection was done on the right side by Dr. Tejal Raju on 14 November 2014.The next morning the pain was in the lower right leg. While making the bed I twisted my body slightly and huge pain switched on up and down the entire leg. This was the most pain I have ever had; it went on an hour or so. Much later in the day the pain was in the lower leg and foot. The right-leg pain persisted for more than two weeks at variable level, often quite excruciating. Dr. Raju prescribed 100 mg of Gabapentin 3 times a day. After taking the pill, the pain subsided somewhat for a few hours and then returned. On 3 December 2014 Dr. Tejal Raju changed my pain medicine from Gabapentin to Tramadol 50 mg every 6 hours; it worked better.
I often have to sit to reduce the pain. I find it difficult to do my regular chores around the house. I cannot walk our dog, which I used to do every day.
Since the epidural steroid injection on 14 November 2014 I have been sleeping in a cushioned Lafuna chair to elevate the knees; this position reduces the leg pain.
Dr. Tejal Raju arranged an appointment with Dr. Caleb J. Behrend at the Carilion Clinic Spine Center (CCSC) in Roanoke on 10 December 2014 to see if a spine operation could be done. He ordered a side x-ray of my spine and said that a date would be set for a lumbar laminectomy. He mentioned that the sudden right-leg pain might be due to rupture of the L4-L5 disc.
About the middle of December 2014 drop foot developed on the right; this has worried me because this sometimes indicates an irreversible situation.
7 January 2015: I had not received an operation date, so I had an appointment with P.A. Allen Crowder at the CCSC. He examined the drop foot and said that an operation date would be set soon.
The Tramadol was not lowering the pain enough, so Dr. Raju put me on Hydrocodone-Tylenol, which worked better but had a side effect of constipation.
About two weeks later I was given a date of 20 February 2015. Even though it was 6 weeks later, I was elated! I asked to be given any earlier date that might open due to a cancellation. Later I received a phone call that the operation date would be 11 February 2015.
I often have stinging pain when I urinate. I have been controlling it by drinking cranberry juice before going to bed. The severe right-leg pain appears to have made the cranberry juice less effective. Eventually, Dr. Hendricks determined that it was not a bladder infection; instead is was a prostate infection. He prescribed Ciprofloxacin.
25 March 2015: Dr. Kevin Griffin looked inside my bladder by catheter and saw no major problem other than a very large prostrate. He put me on Rapaflo and Finasteride, which reduced almost all of the stinging when urinating and allow me to only have to get up twice during sleep.
Early January 2015: I started having difficulty with bowel movement. Either the nerves or the pain medicine or the antibiotic must be the problem. Dr. Hendricks prescribed Colace for stool softening and Senokot-S as a stool-softener and laxative. I quit taking pain medicine and the constipation subsided.
Dr. Tejal Raju ordered another MRI done at Montgomery Imaging Center on 13 January 2015:
MRI L-Spine w/o con
Clinical history: Radiculopathy
Sagittal and axial T1 and T2-weighted images were obtained through the lumbar spine. Alignment is normal.
The L1-2 disc is slightly narrowed and there is very small Schmorl’s node in the superior endplate of L2. There is mild/moderate facet hypertrophy, without spinal or foraminal stenosis.
At L2-3, the disc is relatively well maintained. There is moderate facet and ligamentous hypertrophy, without spinal or foraminal stenosis.
At L3-4, there is severe disc space narrowing. There is annular bulging as well as moderate facet and ligamentous hypertrophy. There is minimal right-sided foraminal stenosis. The let foramen and spinal canal are patent.
At L4-5, there is moderate disc space narrowing and there is a right lateral, subligamentous disc herniation with caudal migration. This is contribution to severe right-sided foraminal stenosis. There is some contribution from the moderately hypertrophied facets as well. The left neural foramen and the spinal canal are patent.
At L5-S1, there is mild annular bulging and moderate facet hypertrophy, without significant spinal or foraminal stenosis.
Impression: Disc herniation on the right at L4-5 with severe foraminal stenosis. Degenerative changes elsewhere as described.
Electronically signed by M.D. Michael R. Aronson on 01/13/2015 at 1118
Reported and signed by: Michael R. Aronson, M.D.
This confirmed the suspicion that the sudden extreme right-leg pain was due to a ruptured disc.
PROCEDURE: MRI imaging was performed at high magnet field strength (3 Tesla). Sagittal T1, T2, STIR, and fat-suppressed T2, and axial T1 and T2 images were obtained through the lumbar spine. 8 cc of Gadavist were administered intravenously without immediate adverse reaction; and sagittal and axial fat-suppressed T1 images were subsequently obtained.
CORRELATIVE STUDIES: MR lumbar spine dated 10/15/14.
FINDINGS: At T12-L1 level, there is no significant posterior disc herniation, spinal canal stenosis, or neural foraminal narrowing.
At L1-L2 level, there is posterior disc bulge/osteophyte complex, ligamentum flavum hypertrophy, and facet hypertrophy, causing mild circumferential compression of thecal sac.
At L2-L3 level, there is posterior disc bulge/osteophyte complex, ligamentum flavum hypertrophy, and facet hypertrophy, causing mild to moderate spinal canal stenosis.
At L3-L4 level, there is approximately 4 mm rightward subluxation of L3 on L4, posterior disc bulge/osteophyte complex, ligamentum flavum hypertrophy, and facet hypertrophy, causing moderate spinal canal stenosis and mild bilateral neural foraminal narrowing.
At L4-L5 level, there is evidence of interval posterior decompression. There is no significant spinal canal stenosis. There is posterior disc bulge/osteophyte complex and facet hypertrophy, causing moderate left neural foraminal narrowing and severe right neural foraminal narrowing. There is evidence of significant interval enlargement of nonenhancing right paracentral disc extrusion extending inferiorly in the right anterior epidural space, causing marked impingement and posterior displacement of descending right L5 nerve root in the right lateral recess.
At L5-S1 level, there is evidence of bilateral L5 pars defects. There is posterior disc bulge/osteophyte complex and facet hypertrophy, causing mild right neural foraminal narrowing.
There is mild reactive marrow edema adjacent to the endplates at L4-L5 level. The visualized marrow otherwise exhibits normal MR signal characteristics.
The distal end of the conus medullaris terminates at the T12-L1 level, which is within normal limits in position.
IMPRESSIONS: Postsurgical changes and multilevel degenerative changes as described. Please see detailed discussion above.
MRI 15 October 2014 |
MRI 13 January 2015 |
MRI 7 August 2015 |
L1-L2: There is disc height loss and diffuse disc bulging. There is facet hypertrophy. The facet hypertrophy is greater on the left which causes mild mass effect on the posterior left side of the thecal sac. Technically, there is no central canal stenosis. There is minimal narrowing of the right foramen. There is mild to moderate narrowing of the entrance of the left foramen mostly due to the facet hypertrophy. |
The L1-2 disc is slightly narrowed and there is very small Schmorl’s node in the superior endplate of L2. There is mild/moderate facet hypertrophy, without spinal or foraminal stenosis. |
At L1-L2 level, there is posterior disc bulge/osteophyte complex, ligamentum flavum hypertrophy, and facet hypertrophy, causing mild circumferential compression of thecal sac. |
L2-L3: There is disc dehydration, disc height loss and diffuse disc bulging. There is facet and ligamentum flavum hypertrophy. There is central spinal canal stenosis, moderate. There is mild bilateral foraminal narrowing. |
At L2-3, the disc is relatively well maintained. There is moderate facet and ligamentous hypertrophy, without spinal or foraminal stenosis. |
At L2-L3 level, there is posterior disc bulge/osteophyte complex, ligamentum flavum hypertrophy, and facet hypertrophy, causing mild to moderate spinal canal stenosis. |
L3-L4: There is marked disc height loss. There is diffuse disc bulging, facet and ligamentum flavum hypertrophy. There is circumferential spinal canal stenosis, moderate. There is right lateral recess stenosis, moderate to severe right foraminal stenosis and moderate left foraminal stenosis. |
At L3-4, there is severe disc space narrowing. There is annular bulging as well as moderate facet and ligamentous hypertrophy. There is minimal right-sided foraminal stenosis. The let foramen and spinal canal are patent. |
At L3-L4 level, there is approximately 4 mm rightward subluxation of L3 on L4, posterior disc bulge/osteophyte complex, ligamentum flavum hypertrophy, and facet hypertrophy, causing moderate spinal canal stenosis and mild bilateral neural foraminal narrowing. |
L4-L5: There is a disc extrusion on the right with disc material extending inferiorly, posterior to the upper margin of the L5 vertebra. There is displacement of the descending nerve roots. Additionally, there is diffuse disc bulging, facet and ligamentum flavum hypertrophy as well as small synovial cyst or associated with the right and left facet joints. These factors combine to cause moderate to severe central spinal canal stenosis. There is severe right foraminal stenosis due to a combination of these factors and mild to moderate left foraminal stenosis. |
At L4-5, there is moderate disc space narrowing and there is a right lateral, subligamentous disc herniation with caudal migration. This is contribution to severe right-sided foraminal stenosis. There is some contribution from the moderately hypertrophied facets as well. The left neural foramen and the spinal canal are patent. |
At L4-L5 level, there is evidence of interval posterior decompression. There is no significant spinal canal stenosis. There is posterior disc bulge/osteophyte complex and facet hypertrophy, causing moderate left neural foraminal narrowing and severe right neural foraminal narrowing. There is evidence of significant interval enlargement of nonenhancing right paracentral disc extrusion extending inferiorly in the right anterior epidural space, causing marked impingement and posterior displacement of descending right L5 nerve root in the right lateral recess. |
L5-S1: There is mild diffuse bulging. This is most prominent at the level the foramen with foraminal stenosis on the right causing some deformity of the nerve root within the foramen and to a lesser extent on the left side. Central canal is not stenotic. |
At L5-S1, there is mild annular bulging and moderate facet hypertrophy, without significant spinal or foraminal stenosis. |
At L5-S1 level, there is evidence of bilateral L5 pars defects. There is posterior disc bulge/osteophyte complex and facet hypertrophy, causing mild right neural foraminal narrowing. |
Impression: |
Impression: Disc herniation on the right at L4-5 with severe foraminal stenosis. Degenerative changes elsewhere as described. |
There is mild reactive marrow edema adjacent to the endplates at L4-L5 level. The visualized marrow otherwise exhibits normal MR signal characteristics. |
http://www.disabled-world.com/artman/publish/spine_picture.shtml:
| L4 | The most likely to herniate (herniated disc, bulging disk, compressed disk, herniated intervertebral disk, herniated nucleus pulposus, prolapsed disk, ruptured disk, slipped disk). The effects of this can cause pain and numbness that can radiate through the leg and extend down to the feet (sciatica). Spondylolysis and spondylolisthesis are conditions that affect the moveable joints of the spine that help keep the vertebrae aligned one on top of the other. Spondylolysis is actually a weakness or stress fracture in one of the bony bridges that connects the upper and lower facet joints. This fracture can happen at any level of the spine but usually occurs at the fourth (L4) or fifth (L5) lumbar vertebra. L4 and L5 fractures are commonly the result of a high impact trauma from falls or motor vehicle accidents. |
| L5 | The fifth lumbar vertebra (L5) is the largest of the five lumbar vertebrae and is considered an atypical vertebra due to its shape. As the last of the lumbar vertebrae, the L5 vertebra bears more body weight than any of the other 23 vertebrae that sit atop it in the vertebral column. The L4 and L5 disc, in between the L4 and L5 vertebrae, can herniate or degenerate, leading to possible leg pain (sciatica) and/or lower back pain. The fifth lumbar vertebra is the most common site of spondylolysis and spondylolisthesis. Sacral Nerves (S1 to S5) injuries generally result in some loss of functionin the hips and legs. Little or no voluntary control of bowel or bladder, but patients can manage on their own with special equipment Most likely they will also still be able to walk. |
After my laminectomy the right-leg pains reduced, but later the pains increased at a lower level than before the operation. An MRI done on 7 August 2015 showed "At L4-L5 level, there is evidence of interval posterior decompression. There is no significant spinal canal stenosis. There is posterior disc bulge/osteophyte complex and facet hypertrophy, causing moderate left neural foraminal narrowing and severe right neural foraminal narrowing. There is evidence of significant interval enlargement of nonenhancing right paracentral disc extrusion extending inferiorly in the right anterior epidural space, causing marked impingement and posterior displacement of descending right L5 nerve root in the right lateral recess." The L4-L5 disc had herniated the second time.
After consulation with my surgeon at which he stated that about 5% of discs that had herniated do it again the 2nd time and that then more recurrent herniation are likely to occur, it was decided that a TLIF operation might be prrformed at some future time. Later the operation date was set for 18 December 2015.
References for Recurrent Lumbar Disc Herniation
After consulation with my pain physician it was decided that a trial of the Nevro Senza SCS would be done. My surgeon agreed that there is low risk for such a trial.
The Nevro Senza SCS system uses two electric leads with 8 eletrodes each that are inserted in the epidural space of the thoracic region of the spinal column. A pulse generator transmits a 10-kilohertz signal to selected electrode pairs on the two leads. If the system works it prevents nerve pain due to spine problems in the lumbar spine from transmitting to the brain. Two different electrodes are excited as electric dipoles for each of 3 programs. There are two intensities: #5: 2.0-milliamps and #6: 2.5-milliamps. The 3 programs and 2 intensities are selected by a wireless remote shown below.
The Nevro Senza SCS system has a trial setup with an external pulse generator and a permanent setup with an implanted pulse generator (IPG).
The trail external pulse generator is attached to a belt::

A small blinking green light in the middle shows that the pulse generator is transmitting to the leads.
A remote, as show below for the permanent SCS, is used for the trial setup.


The components of the Nevro Senza SCS are:
"Leads are placed in the midline epidual space with a staggered offset to cover the target areas in a contiguous fashion. For back and leg pain, the first electrode of one lead is usually placed at the top of the T8 verterbra and the last electrode of the second lead is usually placed at the bottom of the T11 vertebra with some overlap of the leads at the T9/T10 disc. ... These positions have been determined by empirical observations to be effective. The overlap provides some protection against lead migration, which can be especially common during the trial phase. This large span is provided by SCS octopolar leads that have 5-mm spacing between the contact edges. ... After the leads are placed, the impedances are checked to insure the integrity of the stimulation system, and the leads are verified to be in the epidural space before completing the procedure. ... programs involve multiple contacts and typically utilize amplitude between 1 and 5 mA. ... The Senza system has been designed to deliver a safe waveform--a current-controlled pulse delivered at 10,000 Hz. The waveform maintains charge balance, an important aspect of neurostimulation safety."
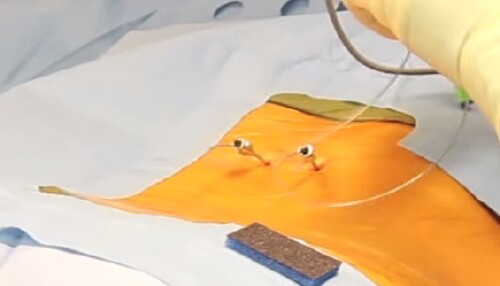 Leads' entry points. |
 Two leads placed in my thoracic thecal sac for the trial. Insertion was at L1. There are 8 electrodes/lead. The right lead shifted down about half its length during the trial. |
 Incision for implantation of the IGP |
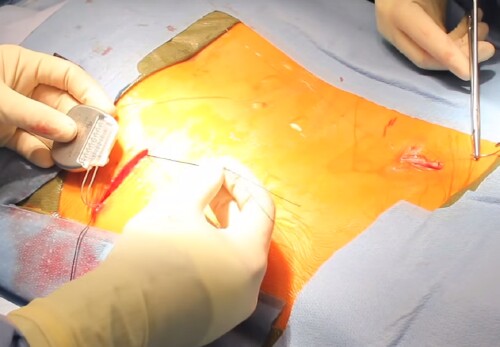 An extension lead under skin connects the 2 leads to the IGP. |
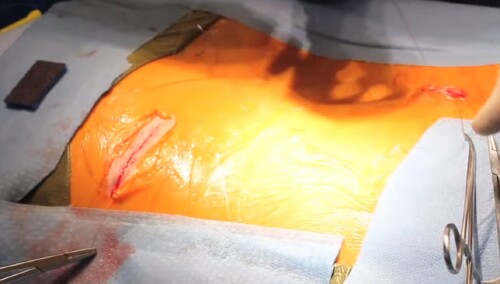 Finish |
https://en.wikipedia.org/wiki/Gate_control_theory:
"Gate control theory asserts that activation of nerves which do not transmit pain signals, called nonnociceptive fibers, can interfere with signals from pain fibers, thereby inhibiting pain. Afferent pain-receptive nerves, those that bring signals to the brain, comprise at least two kinds of fibers - a fast, relatively thick, myelinated "Aδ" fiber that carries messages quickly with intense pain, and a small, unmyelinated, slow "C" fiber that carries the longer-term throbbing and chronic pain. Large-diameter Aβ fibers are nonnociceptive (do not transmit pain stimuli) and inhibit the effects of firing by Aδ and C fibers."
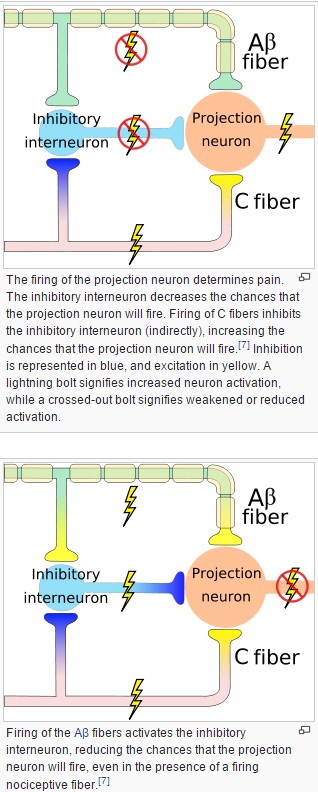
In addition to neuron interaction, there is some indication that neurotransmitters in the synapses between neurons are affected by SCS.
Day |
1 |
2 |
2 Sleep |
3 |
3 Sleep |
4 |
4 Sleep |
5 |
6 |
7 |
Program Intensity |
P1 I5 |
P1 I5 |
P1 I6 |
P2 I5 |
P2 I6 |
P3 I5 |
P3 I6 |
Best |
Best |
Best |
I could not estimate how much pain reduction for the 3 programs with the two intensities per program due to the four pain locations and the complexity of their occurrence. It was later determined that one of the two leads had migrated several vertrae lower. Finally, for a long day another program was used in which the 4 dipole pairs on a lead were excited in a cycle with 20 seconds per pair.
Removal of the lead that stayed in place was painless. Removal of the lead that had migratd involved level-2 pain at the skin.
After removing the trial leads I felt the leg pain level increase as I walked out of the clinic. A day later I estimated that my distributed and complex pains were reduced 50% or more by the SCS.
After reading many web pages about SCS and experiencing the Nevro Senza trial, this slideshow convinced me to have the Nevro SCS instead of a TLIF operation: HFS: Paresthesia Free Back Pain Treatment
A major concern for me is lead migration, since one of my trial leads migrated a large distance: Lead Migration After SCS A 'Universal Problem' I need to learn more about the anchoring of leads during the permanent implanting of the Nevro Senza SCS.
On 17 November 2015 Dr. Chheany Ung implanted a Nevro-Senza Spinal-Cord Stimulator (SCS) (http://www.nevro.com) in me at Carilion Roanoke Community Hospital. It worked out fine except that the procedure time was increased because of some arthritis in my spine.
Two small cylindrical leads, with 8 electrodes at the top of each, were inserted at L1 up into the thoracic spinal canal, and a pulse generator/battery (~2/5-milliampere current at 10-kilohertz voltage pulses between specific electrode pairs) was implanted under the skin of the lower right back and an extension lead under the skin connected the two leads to the pulse generator.
It will take a week or so before I can estimate how much the leg pains are reduced due to the SCS, because the pains due to the two small (~1" & ~3") incisions are being reduced somewhat by an opioid, which also reduces the leg pains.
There is a remote for changing between three stimulation programs, which selects which electrode pairs are activated, and changing the current between six values. I hope that Nevro will develop a smart-phone app as a remote, so that one would not have to take the Nevro remote on trips.
This Nevro SCS was approved by the FDA in May 2015 after being used extensively in Europe and Australia for five years with great success (~70% reduction of leg and back pain). Older methods for SCS used ~50 Hz pulses which "replaced" the pains by buzzing (paresthesia) with less success and more aggravation than the Nevro-Senza method.
There is no sensation due to Nevro Senza stimulation except pain reduction! Of course, there is incision pain at the back L1 location where the two leads were inserted and most severe at the lower right side of the back where the 3" incision was for the insertion of the pulse generator.
I recorded my estimate of legs' pains and minor lower-back pain for a week before the procedure was done to compare to estimates I will make over the next several weeks.
I estimated the pain levels for the four pain locations for the week before the implantation:
Date |
Left thigh |
Right hip |
Right calf |
Lower back |
Walked (Miles) |
10-Nov-15 |
2 |
5 |
5 |
1 |
1.38 |
11-Nov-15 |
1 |
5 |
4 |
3 |
1.31 |
12-Nov-15 |
1 |
5 |
5 |
1 |
1.43 |
13-Nov-15 |
1 |
6 |
6 |
0 |
1.79 |
14-Nov-15 |
2 |
6 |
5 |
2 |
0.72 |
15-Nov-15 |
1 |
5 |
6 |
2 |
1.49 |
16-Nov-15 |
2 |
5 |
6 |
3 |
1.81 |
The SCS schedule for the first days after the SCS implantation on 17 November 2015 was:
Days |
Program |
Intensity |
1-4 |
1 |
4 |
5 |
1 |
5 |
6 |
1 |
6 |
7 |
1 |
7 |
8 |
2 |
4 |
9 |
2 |
5 |
10 |
2 |
6 |
11 |
2 |
7 |
12 |
3 |
4 |
13 |
3 |
5 |
14 |
3 |
6 |
15 |
3 |
7 |
I estimated the pain levels for the four pain locations for the first 15 days after the SCS implantation. Here I show only the estimated pain levels for the two most severe pains in the right hip and right calf:
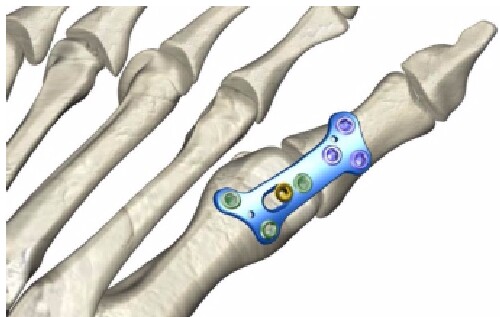
Due to a lawn-mower accident in 1966 that cut of the outer muscle of my right great toe, my right great toe first joint was completely arthritic and it was rigid toward the index tow (Hallux Rigidus). On 25 February 2016 the arthritic bone and remaining cartilage was removed; then the toe was placed in a functional and anatomic position and the joint was fused with a plate and multiple screws (Arthrodesis). Also, the fungal toe nail was removed so a new nail could grow.
Once prepared, the two bones are positioned and a long screw and a metal plate with six screws are placed to hold both bones together. After the hardware is placed, the incision is closed with sutures and the foot is placed in a dressing or splint.
 The right great toe was straighten by a fusion after some arthritic bone was removed.
The fungal great-toe nail was removed. The right great toe was straighten by a fusion after some arthritic bone was removed.
The fungal great-toe nail was removed. |
 |
 |
 |
 |
 |
 I wore this wrap over a plastic for one week. I used a knee scooter for moving. |
 Foot after wrap was removed. |
 Foot after cast was removed. |
 |
 |
 |
http://www.roperld.com/science/RightGreatToeFusion_Before_After.pdf
After surgery a splint was place on the calf and foot; I could not place any weight on the right foot for two weeks. Then my right leg was placed in a cast for 9 days. I used a knee scooter and a walker for mobility.
As instructed I took the bandaging off of the right foot yesterday afternoon. Within a few hours I started having sporadic about 1-second-duration level-5-or-6 stabbing pain in the top of the foot to the right of the scar. I thought that it might be that the tight wrapping was preventing that pain previously, so I put tight wrapping back on, but the pain still occurred. This is by far the most pain I have had since the operation. The foot looks the same as before the pain started. The pain mostly goes away when I walk; it occurs when I sit or lie down.
I thought it might be related to the spinal-cord stimulation, so I turned it off; but, the pain remained. I wonder if it might be some interaction between the L4-re-herniation pain for which I have the spinal-cord-stimulation (SCS) insertion on 17 November 2015.
I took a shower with little difficulty the last two evenings.
I took a 650-mg acetaminophen at 10:30 PM. Then I took a Tramadol at about midnight. Neither helped, so I took the first oxycodone/acetaminophen that you had prescribed at about 1 PM, which might have helped a little, but not much. (Opioids cause me to have hard-to-manage constipation, so I took very little of them after my laminectomy (11 February 2015) and the SCS insertion.)
I had trouble getting to sleep. I think I finally dozed off by about 2 AM, but woke up at 4:45 with steady level-6 pain in the top and bottom of the middle of the foot. I got up and started writing this. I went back to bed to see if I could get some more sleep. I may have slept another hour. I am still having the sporadic pain when sitting or lying down, but not as often and not as severe as last night in bed.
Should I come by to see you today to see if you can figure out the pain problem; or should I see Dr. Tejal Raju, who has been helping me with the L4-herniation pain for the last 1.5 years?
Dave Roper
Dr. Naldo,
I have been thinking some more about the sporadic short stabbing pain on top of my right foot when sitting and lying down that I told you about in my previous message this morning.
In the past when I wore tight shoes I had a similar pain. I wonder if you had to stretch the skin to close the incision. Perhaps there is some arthritis below the skin where the pain is and tightness there causes the pain. Perhaps walking provides a massage action that alleviates the pain.
Dave Roper
 |
 Note the arthritis where the great tumbs join the palm bones. |
 |
 |
 |
 |
Around the year 2000 or earlier I started having numbness on the outside of my left thigh and my left buttock. Gradually it traveled down the leg and often a severe tingling pain would accompany it when standing for a long time or sitting for a long time.
I saw a chiropractor in 2001 and had an x-ray taken of my lower spine. I saw a neurologist in May 2003 and had an MRI of my lower spine. The diagnosis was that I have bilateral spondylolysis at the L5 vertebra (the lowest vertebra on the spine) with mild spondylolisthesis. The L5 vertebra has slipped forward on the sacrum.